Chronic Obstructive Pulmonary Disease (COPD)
Chronic Obstructive Pulmonary Disease (COPD) is a common, preventable condition characterized by progressive, poorly reversible airflow limitation often with systemic manifestations, in response to exposure to tobacco smoke and/or exposure to other harmful inhalational exposures. Smoking, exposure to biomass, occupational exposures, environmental air pollution and tobacco smoke are common risk factors for COPD.
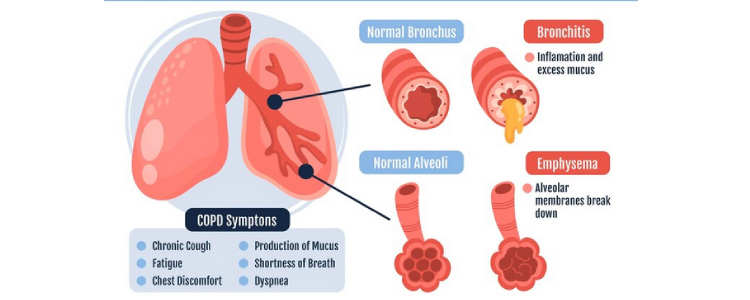
It has large impact on quality of life. In COPD patients there are number of pathological alterations in the lungs.
Exacerbations and co-morbidities contribute to the overall severity in COPD patients. COPD is a major cause of chronic morbidity and mortality throughout the world and vary across the countries and across different groups.
The prevalence of COPD is higher in smokers, ex-smokers compared with non-smokers and in elderly men than women. Worsening of symptoms like cough, breathlessness, increased sputum volume and change in sputum colour [Exacerbations of COPD] account for the greatest burden.
COPD is characterized by slow emptying of the lungs during a forced expiration and there is decline in lung function over time that is variable in individual patients and depending on smoke exposure.
Smoking tobacco is the single most important factor for the development of COPD in addition to occupational exposures, air pollution and respiratory infections etc. They present with breathlessness, activity limitation, chest tightness and cough with or without sputum production. In patients with appropriate clinical history, spirometry confirms the diagnosis of COPD. Unrecognised and under treated COPD can lead to increased morbidity and mortality.
The diagnosis of COPD should be considered in any patient who present with chronic cough with or without sputum production, breathlessness with history of exposure to risk factors for COPD and with typical spirometry findings.
Concomitant comorbidities occur frequently in COPD patients, including cardiovascular disease, metabolic syndrome, osteoporosis, depression, anxiety and lung cancer which should be actively sought and treated appropriately since they influence health status of the COPD patients irrespective of severity of airflow obstruction due to COPD.
In a patient who is known or suspected to have COPD we assess the following: Exposure to risk factors such as smoking, past medical history such as history of airway disease, family history of COPD or other chronic respiratory diseases, history of exacerbations or previous hospitalizations for respiratory disorders, presence of comorbidities, impact of disease on the patient’s life, social and family support available to the patient and possibilities for reducing risk factors, especially smoking cessation.
Smoking cessation is the key. Nicotine replacement and pharmacotherapy reliably increase long-term smoking abstinence rates. Treatment regimen should be individualized to reduce COPD symptoms, reduce the frequency and severity of exacerbations and improve health status and exercise tolerance. We assess inhaler technique regularly.
Vaccination and pulmonary rehabilitation are other key components in the management apart from assessment for need for oxygen therapy, home BiPAP, COPD exacerbation prevention measures and lung transplant assessment in those patients who require it.
Patients with COPD requires comprehensive, personalized care to manage it effectively tailored to the patient needs.